The antiretroviral therapy in Tanga, Tanzania – Medicines and patients between global power structures and local agency
Head of the research project:
Prof. Dr. Hansjörg Dilger
Research associate:
M.A. Dominik Mattes
Laufzeit: 01.09.2008 - 31.08.2010; 01.05.2011 - 30.04.2012
Funding Institution: Fritz Thyssen Stiftung
Finanzvolumen: 1 BAT IIa-Stelle (1/2) sowie Sachmittel in Höhe von 60.000,-- €
Fritz Thyssen Stiftung Jahresbericht 2008/2009 (pdf)
Description
Background
It has only been a few years that the free provision of antiretroviral medicines (ARVs) poses the opportunity for many people living with HIV/AIDS in sub-Saharan Africa to receive treatment for their infection and to resume their everyday lives. In 2004 the Tanzanian Government established its National Care and Treatment Program which by August 2009 provided the life-prolonging drugs to approximately 235.000 patients.
The multiple hopes associated with ARV provision are yet overshadowed by several adverse factors: Restrictions with regard to treatment access and the provision of intensive medical care and long-time control of individual patients make antiretroviral therapy (ART) a medically and logistically challenging issue. The danger of resistant virus strains developing from insufficient patient adherence to the strict treatment regime highlights the necessity for social science research to go beyond the clinical setting and to focus on the intimate linkage of the drugs with the lives of individual patients, their families and their wider social surrounding.

Selection of ARV compounds
Hypotheses
The study assumes that the experiences and actions of ART users and providers are significantly shaped by global political and economic processes, as for example structural adjustment policies, pharmaceutical pricing politics, transnational funding structures and internationally standardized treatment guidelines.
On another level, individual and collective ways of dealing with ARVs need to be understood with regard to specific contexts of kinship based networks of mutual support, widely applied traditional healing practices and a diverse religious landscape that inform the decisions and actions of local actors and simultaneously provide them with space for the renegotiation of existing concepts of illness and healing and for actively dealing with their infection.
Third, the research regards hospitals and treatment centers as potentially conflictive locales where standardized international guidelines and public health concepts are to be translated into well informed patients whose biomedically sound and self-responsible conduct reflects their comprehension and appreciation of knowledge that is transferred by doctors, nurses and voluntary peer educators.
Finally, a close examination of the social relations in which the construction of knowledge about the medicines and the ways of dealing with them are embedded, is considered substantial in order to assess their effectiveness both in medical terms and as stimulators of social change.

Patient files at a Care and Treatment Center
Research questions and objectives
The project investigates the implementation and the effects of antiretroviral treatment programs in urban Tanga, a large city on the shore of the Tanzanian Swahili Coast. It seeks to explore the conditions of establishing access to ARVs and the continuum of living and dealing with the drugs from an individual level to the patients’ social and familial environments and the production of a public discourse about HIV/AIDS. In particular, the project pursues the following goals:
- An examination of public and private health facilities providing ARVs explores the situation of access to the drugs as well as the system put in place to transfer the necessary biomedical knowledge about their intake. The corresponding instructions of how to live with the medicines – encompassing intimate issues such as dietary requirements, disclosure to friends or family members and responsible sexual behavior – highlight the medical staff’s endeavor to produce ‘new’ patients’ subjectivities. Hereby the interaction and communication between patients and medical staff and the prevailing techniques and mechanisms that are established to control ‘deviant’ patients are of special interest.
- The second level focuses on the individual experiences of everyday life with the medicines and the way they are framed within the context of patient biographies. Adopting a socially differentiated approach, the experiences of the “biographical rupture” caused by the physical and social impact of the drugs is explored with regard to the individual patients’ economic living conditions and their positions within social and religious networks. This helps to understand the rationales underlying their decisions and actions, which in some cases oppose the instructions and recommendations of biomedical authorities.
- Third, the effects of ART on the interaction between ARV users and their social environments and the inscription of the drugs into the daily routine of the patients’ families are examined. Hereby the pharmaceuticals’ contribution to the normalization of prior situations of suffering that often posed heavy burdens on existing networks of solidarity is investigated as well as their influence on the patients’ readiness to disclose to others. The questions are pursued if the physical recovery affirms tendencies of hiding the infection, and in how far the involvement in the therapy and the witnessing of the patients’ physical resurrection results in an increased uptake of HIV-testing on the part of people within their surrounding.
- Finally the project analyzes the ways the drugs are represented and discussed in the public media as well as in the meetings of selected HIV/AIDS support groups. The project thus aspires to illuminate if and in which ways public and communal discourses on HIV/AIDS are transformed by the growing availability of the drugs and the resulting “chronification” of the previously terminal disease. The examination of processes of change and their effects on individual and collective life-worlds is expected to contribute to a more thorough understanding of the controversially discussed outcomes of treatment and prevention programs within the frame of Tanzania’s HIV/AIDS policies.

“Exit desk”: After receiving the first supply of ARVs patients are told their next appointment date
Methods
During the one-year field work in urban Tanga (2008-2009) a variety of ethnographic and qualitative research methods were applied:
After obtaining basic quantitative information about the medical facilities involved in ARV provision, the multiple challenges of establishing access to ART were traced by semi-structured interviews with medical professionals as well as participant observation at several treatment centers. Information about the funding structures and rationales of different treatment facilities was collected.
Semi-structured interviews with patients and the participation in support group meetings provided insight into individual experiences of the “biographical rupture” caused by ARVs and the everyday life with the drugs. The respondents were differentiated by gender, age, religious affiliation and social background. Gender-specific differences regarding the perception of getting access to and living with ARVs were explored in focus group discussions.
The social relations within families and the wider social environment of the patients were examined through semi-structured interviews as well as participant observation in individual patients’ homes.
Finally, the analysis of messages and reports of print media, TV and radio broadcasts concerning the life with ARVs was complemented through informal interviews with authors of awareness campaigns and policy makers.

Nurse registering blood specimens
Ethical considerations
Confidentiality and anonymity as well as the absolute transparency of the study towards the participants were core concerns of the study. The names of respondents were changed and any descriptive details that would allow for revealing their identity were excluded from oral and written reports.
Informed consent of the participants was obtained by using a written research statement in English and Kiswahili. Participants were thus informed about the study protocol and the objectives of the research as well as the intended further use of data before participating in an interview or discussion. The participants could withdraw from the study at any stage of data collection and analysis.
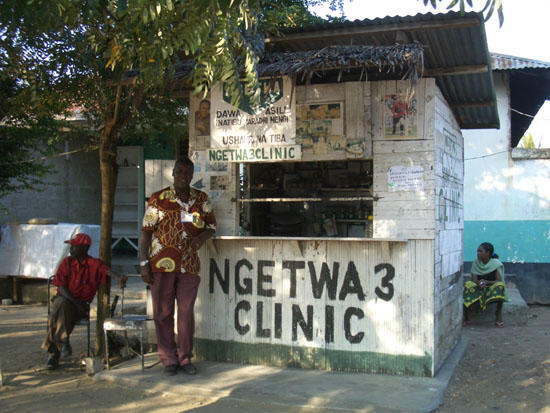
“Dispensary” of traditional herbal medicines